Author: Julie Gros
We spend the majority of our time inside buildings (approximately 87% of our lifetime indoors according to researches [1] ) and ventilation is closely related to the quality and dynamics of air within buildings, which necessarily influences transmission of airborne diseases. Therefore, it is interesting to explore if certain ventilation strategies tend to reduce airborne disease transmission.
As a quick reminder, airborne diseases are diseases that are transmitted through air by any activities which generate aerosol particles or droplets such as breathing, talking, coughing, raising of dust, spraying liquids, etc. Some common airborne diseases are influenza, chickenpox, measles, smallpox, cryptococcosis, tuberculosis and many others. They are part of our daily life, surround us, and concern all of us.
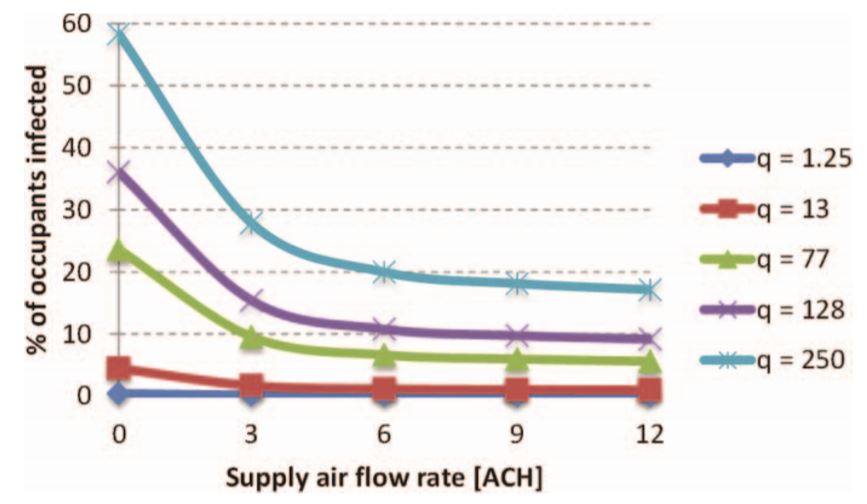
To reduce transmission of airborne diseases, other than the obvious reduction of sources, we can act on the ventilation scheme of the room. The recommendations of the official standards today tell us that increasing ventilation rate is the way to go, and furthermore having a top down ventilation [2] . An interesting study held in Singapore by Pantelic and al [3] showed that increasing the ventilation flow rate up to a certain point is effective in reducing the transmission of diseases, especially for highly infectious ones, in presence of a mixing air delivery system (a system that aims to avoid stratification of the room air).
However, is that always true?
Most of the studies to corroborate this technique were done with strong mechanical ventilation and thus this design strategy may only be applicable to similar situations. Nowadays, there is a significant tendency to go toward reduction of energy consumption for environmental issues resulting in designing energy efficient buildings which are very airtight and have low air velocity design.
In this context and without the strong mechanical ventilation, local air flow patterns are not lost in the chaos. For example, air flow created by heat sources (it can be persons or devices, such as computers or radiators) begins to gain importance in the diminution of personal exposure. One such flow is the human convective boundary layer [4] (CBL), created by the typical warm skin of a comfortable person. When the air around the person skin heats, it flows up, more and more, and finishes in a thermal plume above the person head. According to Licina and al. (2014) [4], considering the CBL, the most favorable air flow patterns are transverse flow from in front and from the side which can even eliminate the exposure at low velocities. Moreover, the CBL is strong enough to influence a person exposure from floor level sources (but not enough to influence the airflow from a cough). A top down ventilation alters the positive effect of this boundary layer. Finally, more is not always better, as increasing the air flow from behind from 0.175 m/s to 0.3 m/s actually increases personal exposure!
What must be remembered is that it is very important to consider the air patterns and sources localization present in the room in order to design efficient transmission reducing ventilation system. Keeping in mind that an ideal strategy for minimizing airborne diseases transmission might not be ideal for other aspects of IAQ (Indoor Air Quality). As always, it is a game of compromises while taking into account the importance of individual criteria on the specific study cases (building category, room geometry, type and location of air supply terminal, obstacles and furniture, number of occupants, etc).

A glimpse into the future?
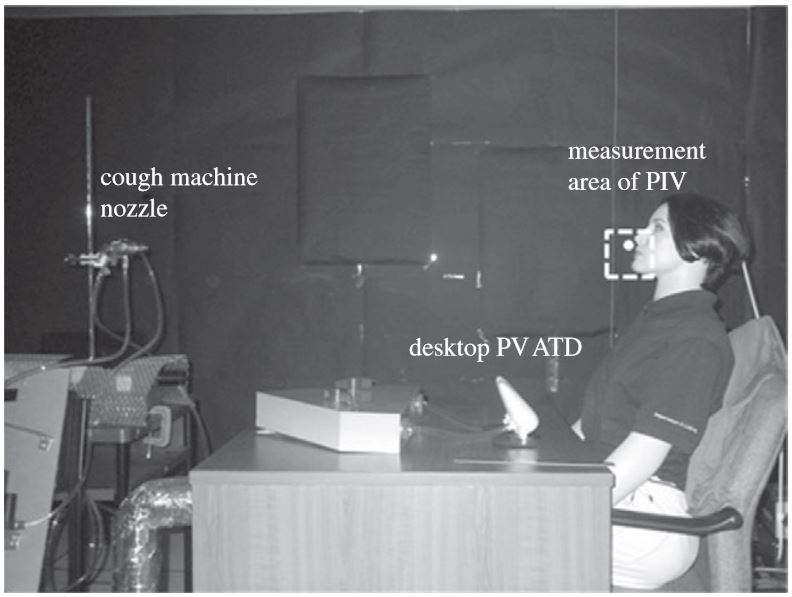
Personal ventilation (PV) might just be what the doctor asked to limit airborne disease transmission. Instead of diluting the total air volume with fresh air to reduce the concentration of pollutants, the method focalizes on the inhalation zone: it creates a clean bubble around the person face. It has been shown by Pantelic and al [5] that DPVATD (Desktop Personalized ventilation Air Terminal Device), essentially a mini air vent on your desktop, could reduce the infection risk from influenza A and tuberculosis by respectively 27% and 65%. This method is ideal in office environment where people’s positions are fixed most of the time and could be associated with a presence detector.
References
1 Klepeis NE, Nelson WE, Ott WR, and al, The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Exp Anal Environ Epidem, 11 (3): 231-52, (2001)
2ASHRAE, HVAC Design Manual for Hospitals and Clinics, Atlanta, Georgia, American Society of Heating, Refrigerating and Air-Conditioning Engineers, (2013b)
2 CDC, Guidelines for Environmental Infection Control in Health-Care Facilities, Atlanta, GA, USA, U.S. Department of Health and Human Services Centers for Disease Control and Prevention, (2003)
3Pantelic J & Tham K.W, Assessment of the mixing air delivery system ability to protect occupants from the airborne infectious disease transmission using Wells–Riley approach, HVAC&R Research, 18:4, 562-574, (2012)
4 Licina D., Melikov A., Pantelic J., Sekhar C. & Tham K. W, Human convection flow in spaces with and without ventilation: personal exposure to floor-released particles and cough-released droplets. Indoor Air 25, 672–682 (2015)
5 Pantelic J., Sze-To G. N., Tham K. W., Chao C. Y. H. & Khoo Y. C. M, Personalized ventilation as a control measure for airborne transmissible disease spread. Journal of The Royal Society Interface 6, (2009).
6 Tang J.W, Noakes C.J, Nielsen P.V, Eames I, Nicolle A, Li Y, Settles G.S, Observing and quantifying airflows in the infection control of aerosol- and airborne-transmitted diseases: an overview of approaches. Journal of Hospital Infection 77, 213–222 (2011)
Featured image : CDC/ Brian Judd, https://phil.cdc.gov/details.aspx?pid=11162