Head and Neck Cancers (HNC) cases approach a million diagnoses each year worldwide. Treatment of HNC involves surgical resection, which is deemed complete if the biopsy comes back from histopathology with clear (negative) margins. Positive surgical margins leave microscopic residues of cancer in the wound bed and require a second resection, as this minimal residual disease in turn gives rise to local and possible non-lac recurrences, and consecutive death of the patient. A positive surgical margin increases the risk of local recurrence by 90%, reducing the overall survival expectancy by 50% and increasing all-cause mortality at 5 years by 90% [1].
Tumor excision with negative margins, i.e., performing resections with clear pathological margins > 5 mm (R0) is the principal aim of oncology surgery. Up to 20% of patients will have a final diagnosis of positive margins despite negative intraoperative margin, due to errors in the sampling of frozen sections (the biopsy is sectioned in 2D sections to be stained and observed under the microscope), analytical error, or resection error due to the patient undergoing reconstruction surgery in between the two resections.
There is a need for a point-of-care method to map the exact tumor margins as a 3D model of the tumor before resection, and detection of residual malignant cells in the wound bed in real-time.
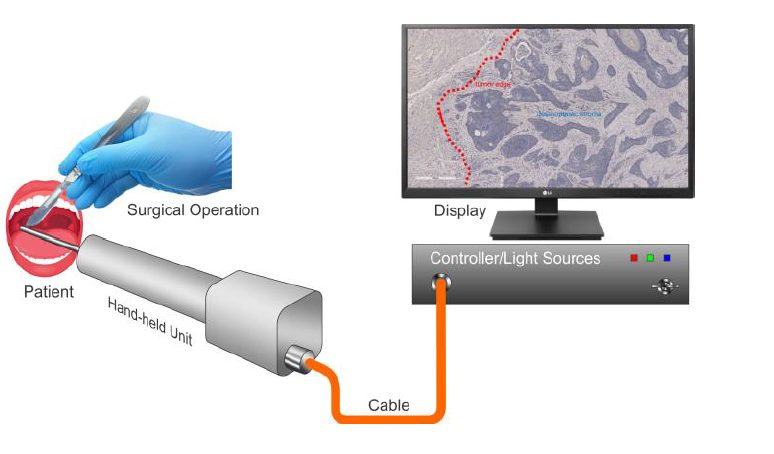
We address this issue by developing a needle-like endoscope, based on a multimode fiber, which allows for deep imaging and diffraction-limited resolution using the transmission matrix method [2,3]. The contrast mechanism is based on endogenous fluorescence of the cells. Tumor cells have a different metabolism as healthy cells, which affects their fluorescent lifetime response [4].
The key technologies linked to this diagnostic are:
– Fluorescence lifetime imaging (FLIM) of endogenous fluorescence, which we know provides relevant information about the cell’s metabolism and allows for a better contrast than solely conventional fluorescence microscopy.
– Machine learning, which allows us to classify normal and tumoral tissues based on their lifetime information.
– Minimally invasive endoscopy, which allows us to probe in deep tissues using a needle-like multimode fiber and reach the >5 mm margin of tissue to observe for the diagnostic.
– Organotypic cell cultures and mouse models to test the probing endoscope and its ability to perform the classification accurately.
This technology can be translated to other cancers, and we believe the endoscope can be useful for monitoring, and delivering light in deep tissues for photodynamic therapies.
Video description of the project and description on the ISREC’s website
Contacts: Victoria Alexandrine Julia Suzanne Marthe Fay and Christophe Moser.