Older adults: Are gait and balance parameters assessed in the lab comparable with those collected in domestic environments?
- Contact person: Arash Atrsaei
- People involved: Arash Atrsaei, Benoît Mariani, Kamiar Aminian
- Partners: Gait Up SA, EPFL, Christian-Albrechts-Universität zu Kiel, Ludwig-Maximilians-Universität München, University of Newcastle, Katholieke Universiteit Leuven, Universidade do Porto, Stichting VU, Motek Medical B.V., Hasomed Hard- und Software für Medizin GmbH, Centre Hospitalier Regional et Universitaire de Lille, Academisch Ziekenhuis Groningen, Patients Know Best
- Funding source: European Union’s Horizon 2020 research and innovation programme under the Marie Sklodowska-Curie grant agreement No. 721577.
Overview:
Gait and balance parameters are most often collected under controlled conditions in the lab or the hospital. These assessments reflect mainly functional capacity, compared to the assessments performed in the home environment that mainly provide information about functional performance. The overlap between functional capacity and functional performance is not yet clearly defined, and for our understanding of daily relevant deficits, a detailed understanding of the degrees of relationships between the respective quantitative parameters of functional capacity and functional performance is indispensable.
To assess the functional capacity and functional performance, we need reliable and accurate tools and algorithms to measure the mobility and balance metrics in both laboratory and domestic settings. Wearable sensors or more specifically inertial sensors provide an objective assessment of gait and balance.
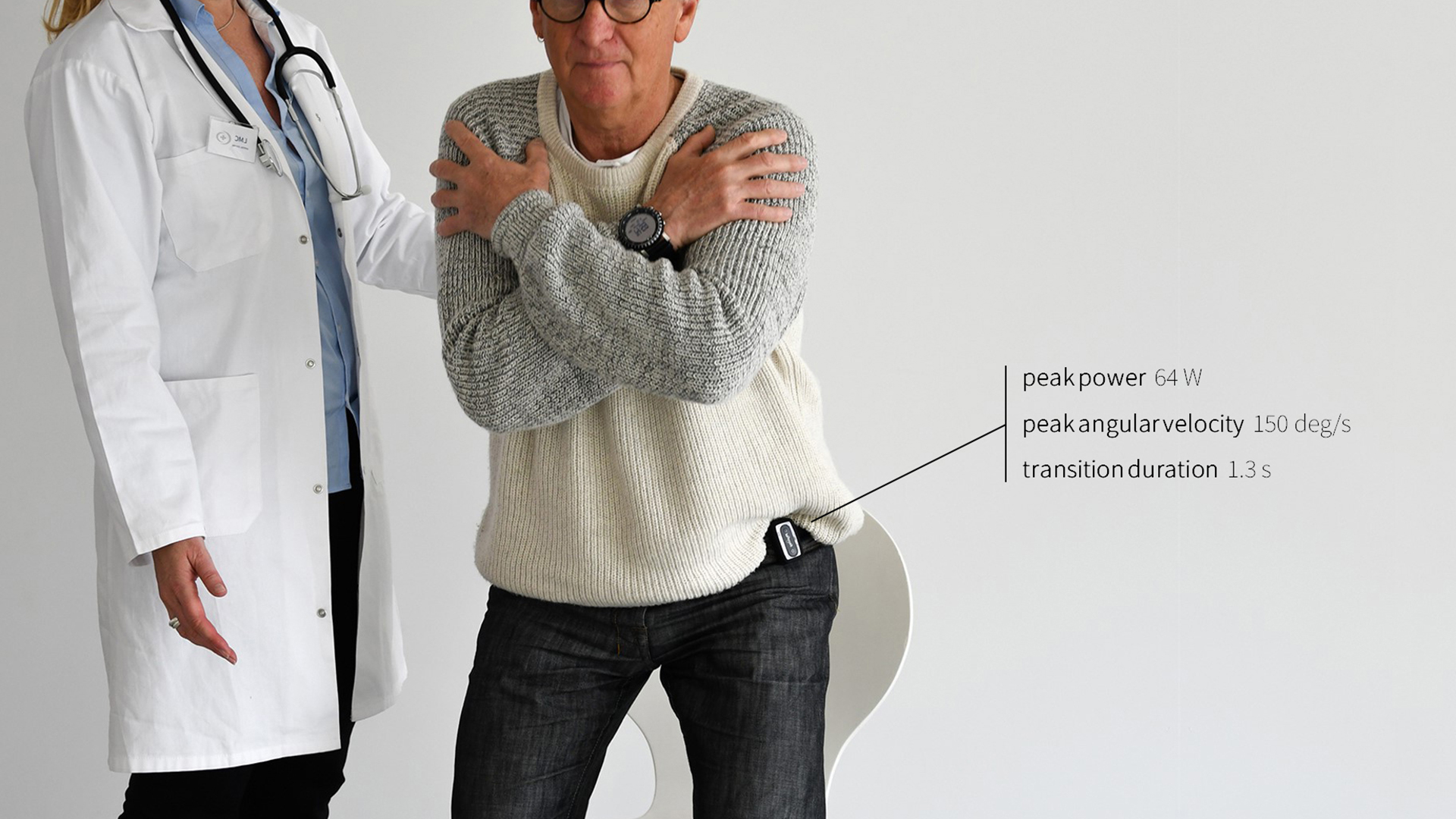
Sit-to-stand and stand-to-sit postural transitions are frequent daily activities which are indicative of muscle power and balance performance. Therefore, detection and analysis of these postural transitions in both clinical and home environments are the key to evaluate the balance performance of the patients.
However, previous works require the attachment of multiple inertial sensors or a single inertial sensor on the body causing discomfort for the clinicians and patients.
Method:
Therefore, our goal is to develop an algorithm based on a single inertial sensor which is capable of detecting the postural transitions in both laboratory and real-life settings and is independent of the location of the sensor around the belt.
Two datasets were used to validate the algorithm. In the first dataset 15 young healthy subjects were recruited and they were asked to perform a five-time sit-to-stand test followed by a sequence of simple daily activities. The second dataset included 43 participant involving healthy younger and older adults, Parkinsonian’s disease patients, patients with multiple sclerosis, and stroke patients performing daily activities in a simulated home-like environment. Participants were video recorder during the whole measurement for later observations.
The detected postural transitions by the proposed algorithm were compared against the video recordings and the performance was reported by the positive predictive value (PPV) and sensitivity (SE) in detecting the sit-to-stand and stand-to-sit transitions.
Results:
For the sit-to-stands the PPV was higher than 97% for the sensors around the belt and the sensitivity was over 90%. For the stand-to-sits the PPV was 93% and above 78% regardless of the location of the sensor.
The performance of the algorithm was the same for different patient populations; however, there was a 10% less accuracy in PD patients.